Leading Experts
in Peritoneal Cancer
Treatments
CYTOREDUCTIVE SURGERY (CRS) ● HIPEC ● PIPAC ● CHEMOTHERAPY ● TARGETED THERAPY ● IMMUNOTHERAPY
Peritoneal Cancer Institute
Peritoneal Cancer Institute is the leading expert center for comprehensive treatment of carcinomatosis in Spain and Europe offering cytoreductive surgery, HIPEC, PIPAC and systemic therapy to treat patients affected by Pseudomyxoma Peritonei (PMP) , appendix and colon cancer, ovarian cancer , mesothelioma or other cancers. #1 medical facility in Spain and Europe providing treatment for complex forms of peritoneal cancer.
We are a high volume dedicated center performing 3 Cytoreductive Surgery with HIPEC procedures a week. Overall more than 170 patients per year receive advanced comprehensive cancer treatment, including not only cytoreductive surgery and HIPEC but also PIPAC (pressurised intraperitoneal aerosolized chemotherapy) and systemic oncologic therapy.



Leading doctors
-

Director, Peritoneal Cancer Institute
Medical director, Peritoneal Surface Malignancies Program, Centro Medico TeknonDr. Sabia is a renowned specialist in surgical oncology, and an expert in the treatment of peritoneal carcinomatosis. He completed his surgical training in 2008 in Italy and joined the Peritoneal Oncology Surgery Unit (UCOP) in Barcelona at the end of 2008, after training in cytoreductive surgery at the Reina Sofia University Hospital in Córdoba, at the National Cancer Institute in Milan and later at the Washington Cancer Institute with Dr. Paul Sugarbaker.
His areas of interest also include open and minimally invasive colorectal cancer surgery, laparoscopic surgery and PIPAC (Pressurized IntraPeritoneal Aerosol Chemotherapy).
-
2002 – 2008
General Surgery Residency
Department of General and Transplant Surgery
Hospital Universitario Reina SofíaDepartment of General and Emergency Surgery
Second University of Naples -
2009 – 2014
Attending Surgeon in Peritoneal Surface Malignancies Surgery
Hospital de la Santa Creu i Sant Pau
Educational stay, Center for Gastrointestinal Malignancies. Program in Peritoneal Surface Oncology
MedStar Georgetown University Hospital, Washington D.C., U.S.A -
2010 – 2021
Attending Surgeon ,Peritoneal Surface Malignancies Unit
CSI, Hospital Sant Joan Despi Moisés Broggi, Barcelona -
2021 – present
Senior Attending Surgeon, Peritoneal Surface Malignancies Unit
CSI, Hospital Sant Joan Despi Moisés Broggi, Barcelona
Director, Peritoneal Cancer Institute
Teknon Medical Centre, Quironsalud Hospitals Group
-
-

Co-director, Peritoneal Cancer Institute
Chief, Peritoneal Surface Malignancies Unit, Consorci Sanitary IntegralDr. Bijelic is an internationally recognised expert in cytoreductive surgery and peritoneal surface malignancies. She has completed her general surgery residency in Washington DC followed by a subspecialty in surgical oncology and peritoneal surface malignancies. Dr Bijelic continued as an attending surgical oncologist with Dr Sugarbaker, a pioneer in the field, at the Washington Cancer Institute before founding a peritoneal surface malignancies program at Inova Schar Cancer Institute. Since 2021, she is the head of the peritoneal surface malignancies unit in Barcelona.
Dr Bijelic has served on committees dedicated to peritoneal surface malignancies in both American and European leading cancer societies and is the academic coordinator of the European School of Peritoneal Surface Oncology. She is certified by the American Board of Surgery.
Dr Bijelic is an active clinical researcher who has published numerous articles and lectured internationally.-
2007 – 2015
Attending surgeon
Washington Cancer Institute, Washington DC, USA -
2015 – 2019
Section Chief , Surgical Oncology
Inova Fairfax Hospital/Inova Schar Cancer Institute -
2019 – present
Co-lead, Peritoneal Oncology Surgery Unit
Hospital Sant Joan Despi Moisés Broggi, Barcelona -
2021 – present
Chief, Peritoneal Oncology Surgery Unit
CSI, Hospital Sant Joan Despi Moisés Broggi, Barcelona
Co-director, Peritoneal Cancer Institute
Teknon Medical Centre, Quironsalud Hospitals Group
-
-

Clinical Oncologist
Within Medical Oncology, his area of specialization is the systematic treatment of tumors of the digestive tract (esophagus-gastric, colorectal, pancreatic, bile duct, liver, small intestine, peritoneal and anal canal) and tumors of the endocrine area (thyroid, gastroenteropancreatic neuroendocrine, paragangliomas, pheochromocytomas, adrenal carcinoma, and tumors of other origins of neuroendocrine lineage).
Active member and participant in different projects in the European Organisation for Research and Treatment of Cancer (EORTC), the European Society for Medical Oncology (ESMO), the European Neuroendocrine Tumor Society (ENETS), the American Society of Clinical Oncology (ASCO), the Multidisciplinary Spanish Group of Digestive Cancer (GEMCAD) and the Spanish Cooperative Group for Digestive Tumor Therapy (TTD).-
2002 – 2006
Medical Oncologist
Hospital de la Santa Creu i Sant Pau -
2006 – present
Medical Oncologist
Vall d'Hebron University Hospital -
2006 – present
Clinical oncologist
Institute of Oncology, Hospital Quirónsalud Barcelona -
2013 – present
Head of Gastrointestinal and Endocrine Tumor Unit
Teknon Oncology Institute
-
Diagnosis
Gastrointestinal cancers are malignant tumors affecting the abdominal digestive organs: stomach, pancreas, liver, small and large intestines or the appendix. Gynecological cancers affect the female reproductive organs such as the ovaries or the uterus. Both gastrointestinal and gynecological cancers can spread to other organs or parts of the abdominal cavity, including its inner covering layer called peritoneum.
When the malignant process involves the peritoneum, this is called peritoneal carcinomatosis, which is one of the rarest and most difficult cancer diagnoses. The peritoneum covers all organs of the abdominal cavity as a thin layer.
The goal of the treatment of carcinomatosis is to surgically remove all tumor deposits whenever possible using an advanced surgical procedure called Cytoreductive surgery. This surgery is combined with the delivery of heated chemotherapy solution into the abdomen to treat the microscopic deposits of cancer and is called HIPEC. In patients who are not candidates for cytoreductive surgery , another procedure to deliver chemotherapy into the abdomen using minimally invasive techniques may be helpful, called PIPAC.
While some types of cancers that may cause carcinomatosis are common, such as colon cancer others are rare, such as pseudomyxoma peritonei and mesothelioma and are best treated in a specialized center for peritoneal cancers.

Types of cancers which can lead to peritoneal carcinomatosis and could benefit from Cytoreductive Surgery and HIPEC:
-
Pseudomyxoma Peritonei (PMP)
PMP is a rare disease characterised by the accumulation of mucinous tumor deposits throughout the abdominal cavity. The malignant process typically starts with a mucinous tumor of the appendix called LAMN (low grade mutinous appendix neoplasm) or HAMN (high grade mutinous appendices neoplasm). This type of carcinomatosis does not respond to conventionally chemotherapy and its main form of treatment is cytoreductive surgery with HIPEC
-
Appendix cancer
The appendix is a thin pouch that is attached to the large intestine located in the lower right part of the abdomen. Appendix cancer which is very rare, occurs when cells in the appendix change, start growing significantly and spreading outside of the appendix. Appendix cancer has a high likelihood of causing peritoneal carcinomatosis. There are different types of appendix cancers that require different approaches to treatment such as mucinous tumors of the appendix, carcinoid ( neuroendocrine) tumors of appendix, appendix adenocarcinoma, Goblet cell carcinomas and others.
-
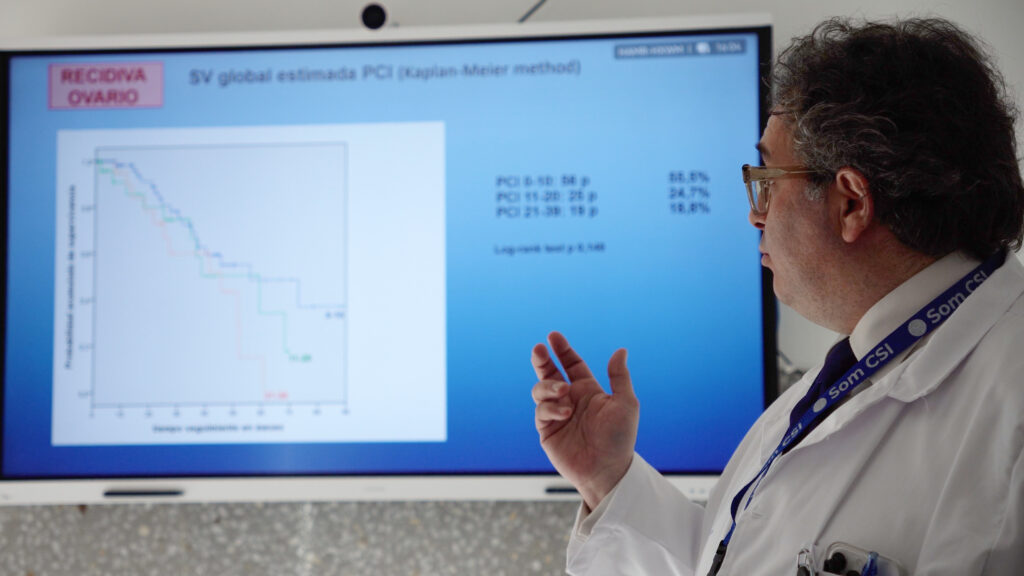
Ovarian cancer
Ovarian cancer is the growth of abnormal cells that form in the ovaries or the fallopian tubes. The cells multiply quickly and can invade and destroy healthy body tissue. Peritoneal carcinomatosis can happen when cancer cells from the ovary spread to the peritoneum.More than half of patients with ovarian cancer will develop carcinomatosis.
-
Colorectal cancer
Colorectal cancer is a type of cancer that begins in the large intestine (colon) or its final part, the rectum.
Colorectal cancer typically affects older adults, but it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon.
Over time some of these polyps can become colon cancers. -
Mesothelioma
Malignant peritoneal mesothelioma is a rare type of cancer that arises from the peritoneum itself. Malignant deposits are often widespread through the peritoneum and produce liquid called ascites. In some patients, prior exposure to asbestos may be linked to the development of mesothelioma.
-
Gastric cancer
Gastric cancer is a growth of abnormal cells that starts in the stomach.
Peritoneal metastasis is one of the most common forms of metastasis in gastric cancer.
It is found in up to 14% of newly diagnosed gastric cancer patients and is also the most common site (~50%) of recurrence in gastric cancer patients after radical surgery. -
Other types of cancer
Many other types of cancer can cause carcinomatosis such as endometrial cancer, small bowel cancer, hepatobiliary and pancreatic cancers, neuroendocrine tumors and others. In selected cases, they may be considered for treatment with cytoreductive surgery and HIPEc or with PIPAC.

Disease evaluation:
-
Symptoms and physical examination
In general, peritoneal carcinomatosis does not cause specific symptoms during the initial stages. For this reason, it is important that patients with advanced tumors and/or suspected peritoneal metastases be referred early to specialized units. In those cases in which the peritoneal involvement by cancer is more advanced, it can produce:
- Abdominal pain.
- Increased abdominal girth.
- Accumulation of fluid in the abdomen (ascites).
- Intestinal obstruction.
-
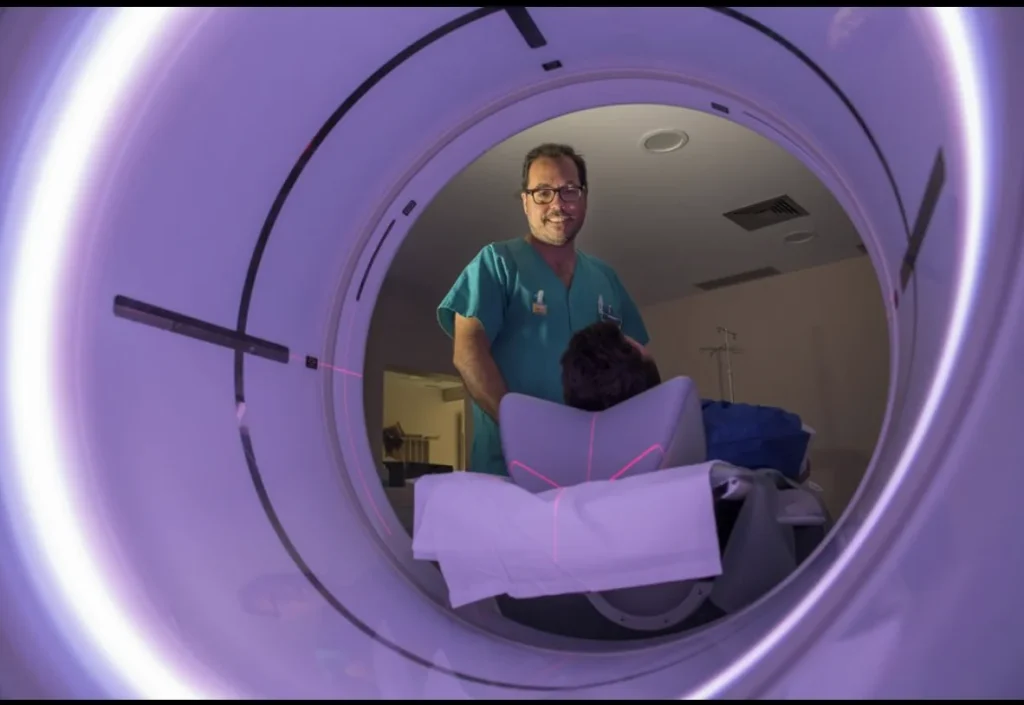
Computer tomography (CT-scan)
It is a medical test that reproduces multiple images of the inside of the body, using X-ray.
With the help of CT, it is possible to see the spread of the tumor with or on the surface of abdominal organs when metastasis reach a size of about 1 cm. To detect smaller metastases on the peritoneum, a diagnostic laparoscopy is often recommended. -
Peritoneal MRI
A technique for obtaining images of anatomical sections of the body using magnetic resonance.
For patients with peritoneal carcinomatosis, dedicated peritoneal MRI protocols are used. The images must be evaluated by an appropriately specialized radiologist. -
PET-СT scan
This technique can be sometimes used instead of a CT scan as it combines computed tomography with intravenous administration of a radiopharmaceutical. It Allows doctors to see the metabolic activity of tumor cells, which can help determine the site of metastasis and provide staging of the disease. Some tumors, such as PMP or other mutinous tumors do not have a high level of metabolic activity and therefore PET scan is not very useful in their evaluation.
-
Diagnostic laparoscopy
Laparoscopy is a type of surgical procedure that allows a surgeon to access the inside of the abdomen and pelvis without having to make large incisions in the skin. This procedure is also known as keyhole surgery or minimally invasive surgery.
Laparoscopy can be used for diagnostic purposes, it allows doctors to determine the extent of tumor spread as accurately as possible before cytoreductive surgery (CRS).
When using laparoscopy to determine if a patient is a good candidate for cytoreductive surgery, the laparoscopy procedure should be done by a surgical team highly specialized in peritoneal carcinomatosis treatment. -
Biopsy and histological analysis
During the operation, doctors perform a biopsy (take samples of tumor tissue) for subsequent histological analysis, which allows them to confirm tumor details such as the histologic subtypes, whether or not lymph nodes are involved and sometimes to perform additional molecular analysis that may help select drugs for systemic oncological treatment following surgery.
-
Other diagnostic tests
Blood tests, electrocardiogram, radiography and other diagnostic methods can be used for a comprehensive assessment of the patient's body condition and are typically done before the scheduled surgery.
Treatment
-

Cytoreductive Surgery (CRS) with HIPEC
Sugarbkaer procedure, Surgery method developed by Dr. Paul Sugarbaker (USA), the purpose of which is to remove all the peritoneal tumor deposits. The extent of surgery will depend on the number and distribution of the tumor deposits that the surgeons encounter. Due to the complexity of this surgery, it should only be performed by surgeons highly specialized and experienced in this procedure.
Once the tumor deposits are surgically removed, the surgical team administers HIPEC ( heated intraperitoneal chemotherapy). During this part of the procedure, the abdomen is filled with heated chemotherapy solution and circulated with the help of a specialised device for 60-90 minutes, which is used to treat the microscopic residuals of the tumor and achieve a better result.
-

Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC)
PIPAC is a novel procedure that allows surgeons to treat the abdominal cavity with chemotherapy in aerosol (gas) form. This procedure is performed through a minimally invasive laparoscopic approach. PIPAC treatment can often be repeated several times to maximise the anti-cancer effect. PIPAC is usually indicted in patients who are not candidates for the CRS HIPEC procedure because their tumor cannot be removed surgically.
-

Systemic oncological treatment
Systemic oncological treatment consists of chemotherapy or immunotherapy administered by vein or in pill form. It can be used in preparation for surgery to make the tumor smaller and reduce surgery volume, or in the postoperative period to help maintain the results and reduce the chance of tumor recurrence.
-
Surgery Complications & risks
-
Hospital stay
-
Follow up
Hospital
The Peritoneal Cancer Institute operates at the clinical base of the Teknon Medical Centre, one of the largest multidisciplinary hospitals in Spain, which allows the patient to receive any necessary medical care and provide the necessary care and supervision in the postoperative period. The hospital regularly undergoes international certification and has been certified by Joint Commission International seven times, which guarantees the high quality and safety of medical services.
The hospital employs more than 400 doctors and 2,000 specialists, providing the best medical care for more than 60,000 patients a year.
The versatility of the clinic allows to treat any complications in the postoperative period and comprehensively approach the restoration of the patient's condition, including the preparation of an individual diet and physiotherapy.
The leading European hospital companies, the German Helios (belonging to Fresenius) and the Spanish Quironsalud have reached an integration agreement that resulted in the creation of the first European operator and one of the most important in the world. The new group will have more than 100,000 employees, will manage 155 health centers, and will maintain both brands, Quirónsalud in Spain and Helios in Germany.
The commitment to top-quality health care, and the commitment to research and patient care as a fundamental axis, have been the hallmarks of both groups and will continue to be those of the new European leader in the sector.
Articles
Show moreFor patients
Support on each step of your treatment
-
Request a free evaluation
Our medical assistant will contact you to find out how we can help you. They will help prepare your case for a consultation with the doctors.
-
Prepare your medical reports and scans
Send your medical reports, CT & MRI scans to your assistant and he will review them and prepare them for the doctors. So no detail is missed.
-
Get an online consultation with the Doctors
Consult with doctors without leaving home. Your assistant will arrange a video call with the Doctors to discuss your treatment plan and receive an official medical report.
-
Prepare for your trip and receive treatment
Once you have made a decision about treatment, our medical assistant will prepare a budget and help organize your visit. The clinic provides visa support.
-
Treatment & hospital stay
Hospitalization in a comfortable individual room on the ward with Barcelona city views. Daily control visits by doctors, a nutritionist, and round-the-clock medical supervision.
-
Follow-up after treatment
We stay in touch with you even after your return home and control the result of treatment. You can always ask questions to your doctors.
Testimonials
FAQ
Cytoreductive Surgery and HIPEC:
-
Cytoreductive Surgery with HIPEC can cure patients, especially those with appendix cancer , PMP, some forms of mesothelioma and ovarian cancer even when there is a large amount of tumor in the abdomen at the time of diagnosis. For other tumors, such as colon cancer and gastric cancer, the CRS HIPEC treatment is applied when there is more limited amount of tumor in the abdomen to achieve the best results. For all tumors that develop peritoneal metastasis, a chance for cure is only possible if surgery ( CRS HIPEC) can be included as part of the treatment.
-
In most cases, both HIPEC and systemic chemotherapy are required for achieving the best results.
The methods are complementary and do not replace each other. Some kinds of tumors, such as PMP, do not benefit from systemic chemotherapy and therefore CRS and HIPEC is the only treatment patients receive. -
Many factors need to be evaluated before the decision to recommend CRS and HIPEC is made and also to determine the prognosis once surgery is done. The type of primary tumor ( such as apendix, colon, ovary, mesothelioma etc. ) and the amount of the peritoneal metastasis that are present are some of the most important factors. Peritoneal carcinomatosis index (PCI) is used to describe the amount of tumor present in the abdomen. Computed tomography (CT), MRI and or diagnostic laparoscopy can be used to estimate the PCI before surgery, but the final assessment is done during surgery. The intraoperative PCI as well as the CC score ( a description of the completeness of the surgical removal of the tumor) are important to determine prognosis after surgery.
-
Like any major surgery, CRS has certain risks, such as bleeding, infection, and the need for reoperation.
Specialised centers are able to maintain the risk of serious complications relatively low, less than approximately 10-15%. The risk of mortality after surgery in specialized centers is also low, less than 2%. Minor complications and side effects are more common and generally happen in about a third of the patients. -
Cytoreductive surgery with HIPEC is a complex surgical intervention that can take as many as 14 hours or more, depending on the extent of the operation and the general condition of the patient. The average duration including the HIPEC is approximately 7 hours.
-
The total period of hospitalization can typically range from 1 to 3 weeks and will depend on the extent of the surgery that was needed in each case. The first 1-2 days, the patient is monitored in the intensive care unit, after which he is transferred to an individual room on the ward. Patiens are encouraged to be out of bed and ambulate during the postoperative period and often receive nutritional support until they are able to recover their dietary intake.
Pressurized intraperitoneal aerosol chemotherapy (PIPAC)
-
The indications and technique for the PIPAC technique is completely different from CRS HIPEC. PIPAC is generally recommended in patients who are not candidates for CRS HIPEC. PIPAC patients are treated with intraperitoneal chemotherapy but the tumor deposits are not surgically removed. During PIPAC, the the chemotherapy drug is administered into the abdominal cavity as an aerosol, in contrast to HIPEC, when the drug is administered in the form of a liquid.
-
The indications and technique for the PIPAC technique is completely different from CRS HIPEC. PIPAC is generally recommended in patients who are not candidates for CRS HIPEC. PIPAC patients are treated with intraperitoneal chemotherapy but the tumor deposits are not surgically removed. During PIPAC, the the chemotherapy drug is administered into the abdominal cavity as an aerosol, in contrast to HIPEC, when the drug is administered in the form of a liquid.
-
PIPAC is less toxic than HIPEC and is used when cytoreductive surgery with HIPEC cannot be performed due to disease progression or the patient's condition.
-
PIPAC is administered using a minimally invasive laparoscopic approach.
-
Compared to CRS, the procedure is much faster and takes 1 - 1.5 hours.
-
Due to the characteristics of the intervention and the use of a minimally invasive approach, the patient’s recovery is much faster and the hospitalization typically lasts 1-2 days in a regular ward.
General questions
-
Yes, a high-calorie, high-protein diet is recommended in preparation for surgery to prepare the body for the post-op period and faster recovery.
In the postoperative period, an individual diet will be compiled for the patient, depending on the extent of the operation and his condition. -
Yes, it is recommended to stop chemotherapy 2-6 weeks before CRS HIPEC surgery and approximately 2 weeks before PIPAC. The exact duration will be determined by your surgeons and coordinated with your oncologist. It may also be necessary to stop other drugs before surgery, such as anticoagulants.
-
Usually, follow-up diagnostics are carried out every 3-6 months: computed tomography (CT), laboratory tests and physical exams. The follow up schedule is coordinated with the patients’ referring physicians . If your condition changes between the scheduled follow up appointments, you should consult your doctor.
For doctors
Peritoneal Cancer Institute collaborates
with doctors and clinics around the world to share knowledge and experience in the fight against peritoneal cancer.
The Institute is included in the list of training centers of the European School of Peritoneal Surface Oncology and the European Society of Surgical Oncology, ESSO.
Having completed the training program at our Institute, surgical specialists receive special skills that allow them to effectively perform cytoreductive operations.
If you are a medical professional interested in cooperation, please fill out the form and we will contact you as soon as possible.